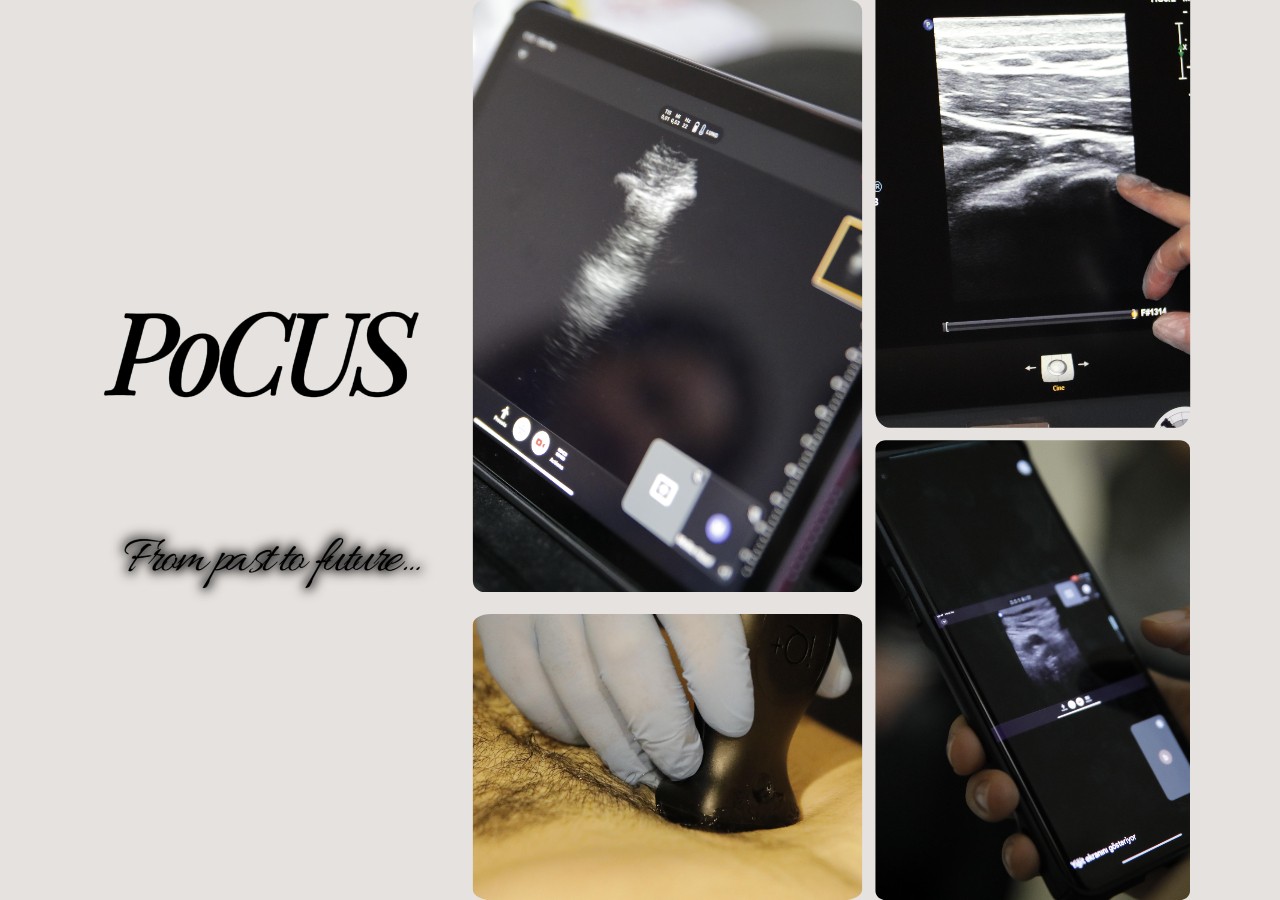
In today’s medical practice, the dizzying pace of technological advancement constantly redefines patient care standards. One of the most innovative approaches in recent years, PoCUS (Point-of-Care Ultrasound), has become an indispensable tool for physicians. By accelerating medical decision-making and improving care quality, it represents a true revolution. But what exactly is PoCUS? When and how did it enter clinical practice? Why is it so important for clinicians, and what concrete benefits has it brought to patient care recently? Most importantly, what does the future hold for PoCUS? Let’s explore these questions together.
What is PoCUS? A Guide to Instant Diagnosis and Treatment
At its core, PoCUS refers to goal-directed ultrasound performed by the clinician directly involved in the patient’s care, at the point of need—whether at the bedside, outpatient clinic, ambulance, or emergency department. This method reduces dependence on radiology departments and allows clinicians to quickly answer their own clinical questions, perform dynamic evaluations, and instantly integrate findings with other clinical data. As a result, diagnoses and treatments become faster, patient safety improves, and unnecessary tests can be avoided. Ultimately, cost-effectiveness is one of the key considerations in modern healthcare.
Timeline of Clinical Adoption and Development
While ultrasound entered the medical world as early as the 1940s, the concept and widespread use of PoCUS is relatively recent. Its emergence in clinical settings began in the 1960s. However, the most transformative progress came in the 1990s, when ultrasound machines became smaller, more portable, and capable of delivering better image quality.
During this period, PoCUS started to gain traction in high-stakes environments such as emergency medicine and intensive care. For instance, in 1994, it was incorporated into emergency medicine training curricula in the United States. Applications like the FAST exam in trauma, identifying reversible causes during cardiac arrest, and guiding vascular access procedures helped PoCUS secure its role in clinical practice. Over time, it expanded into anesthesiology, internal medicine, family medicine, pediatrics, and even medical school education, thanks to simpler user interfaces, compact devices, and improved training opportunities.
PoCUS for Clinicians: As Valuable as a Fifth Limb
PoCUS provides countless benefits for clinicians:
- Rapid and Accurate Diagnosis: Enables immediate confirmation or exclusion of differential diagnoses at the bedside, such as detecting pleural effusion, pneumothorax, or cardiac tamponade within seconds in a patient with acute dyspnea.
- Enhanced Clinical Decision-Making: Real-time imaging supports informed and timely treatment strategies—like assessing fluid responsiveness or monitoring cardiac function in septic shock.
- Increased Safety and Success in Procedures: Ultrasound guidance significantly reduces complications and boosts success in procedures like central line placement, paracentesis, thoracentesis, or nerve blocks.
- Patient Safety and Comfort: As a non-invasive, radiation-free method, PoCUS eliminates the need for transport to imaging departments—saving time, increasing comfort, and avoiding transfer-related complications.
- Understanding Pathophysiology: Its dynamic nature allows for a deeper understanding of disease processes and more personalized treatment planning.
Recent Contributions to Patient Care
PoCUS has made undeniable contributions to patient care. Studies show it reduces length of stay in emergency departments, facilitates quicker interventions for critical patients, and can even reduce mortality in certain cases. For example, identifying the etiology of shock (cardiogenic, hypovolemic, or obstructive) at the bedside enables life-saving treatment without delay. In rural or resource-limited areas, where access to advanced imaging is restricted, PoCUS serves as a ‘pocket stethoscope’ offering crucial diagnostic insight. During the COVID-19 pandemic, its role in quickly evaluating and monitoring lung involvement was pivotal.
Why Should You Take a PoCUS Course?
Despite these impressive advantages, effective, safe, and accurate use of PoCUS depends on structured training. It’s not just about knowing how to operate the device—it’s about understanding what clinical questions to ask, how to interpret images, and how to incorporate this information into comprehensive patient care. That’s why PoCUS courses provide not only technical skills but also enhance clinical reasoning and decision-making.
With structured curricula, simulation-based training, and experienced instructors, PoCUS courses help solidify learning, boost clinician confidence, and improve patient safety. Certified training also supports professional development. For today’s and tomorrow’s doctors, carrying only a stethoscope is no longer enough—it’s time to ‘see, think, and decide’ through imaging. PoCUS courses are among the most powerful tools driving this transformation.
Why ULTIMATE?
Harnessing the full potential of PoCUS requires high-quality education. That’s where ULTIMATE comes in—with a nationally recognized curriculum, hands-on training model, and experienced faculty, it’s a trusted reference point for PoCUS training. ULTIMATE equips clinicians with real-world skills aligned with true clinical scenarios. It’s more than a course—it’s a learning community that supports continuous professional growth.
If you’re ready to become part of this powerful network and elevate your PoCUS skills, we invite you to join ULTIMATE courses.
Assoc. Prof. Dr. Bora Çekmen